Carpal Tunnel Syndrome
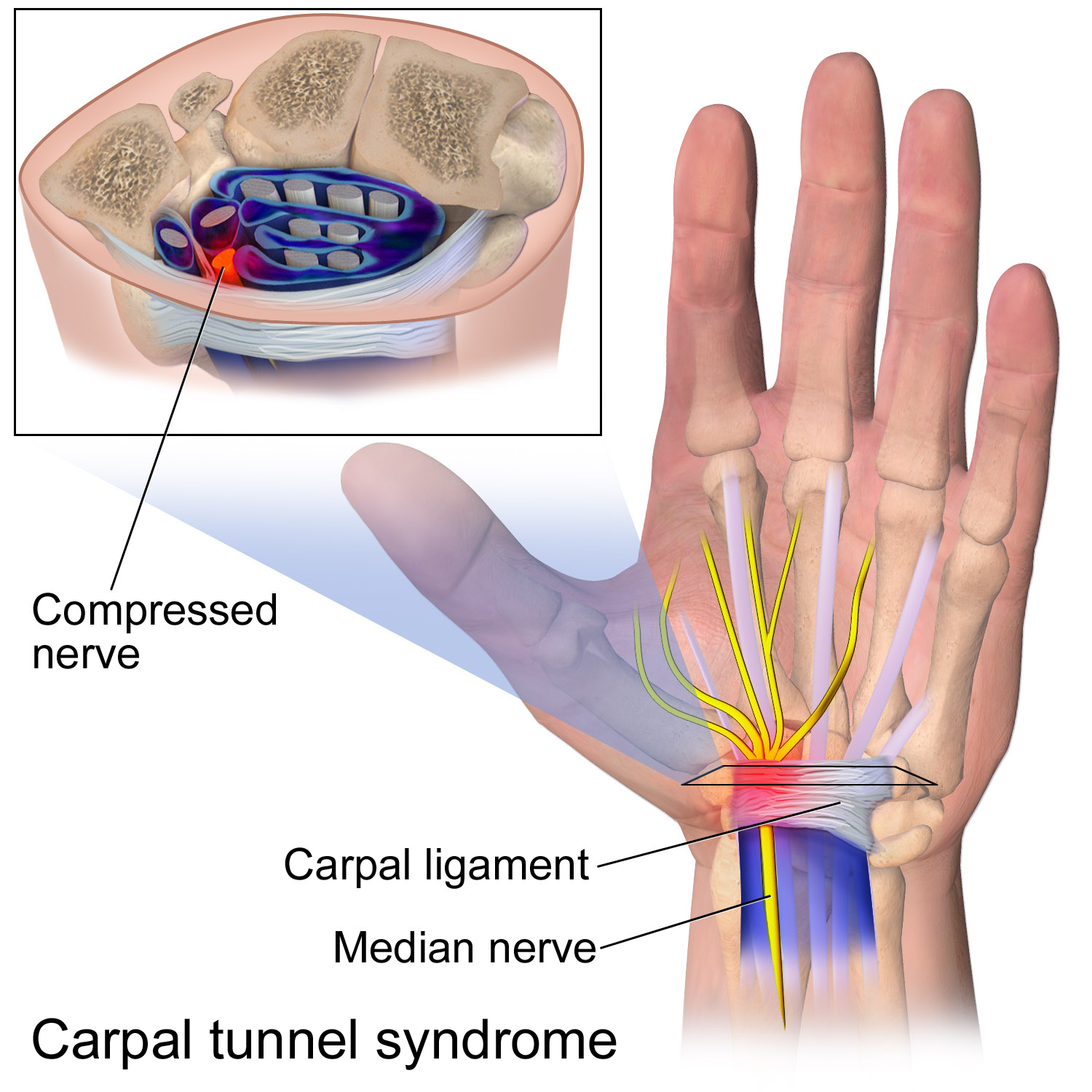
WHAT IS THE CARPAL TUNNEL?
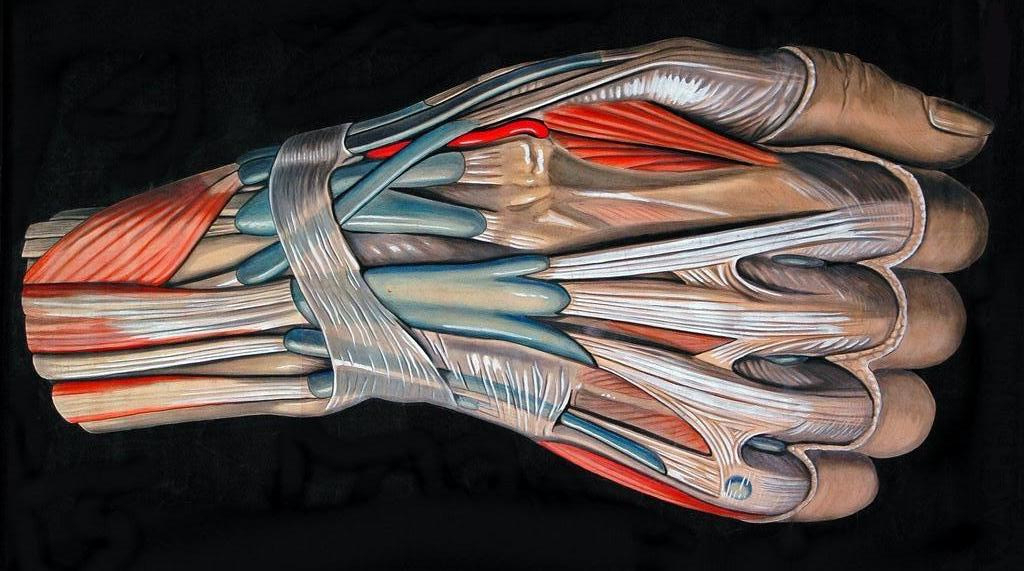
Carpal tunnel syndrome corresponds to compression of the median nerve through the wrist. This nerve provides sensation to the thumb, index, long and half of the ring finger. It is also responsible for innervating the muscles of the base of the thumb. The carpal tunnel is an anatomical zone between the carpal bones and the annular carpal ligament. The median nerve passes through this channel accompanying the 9 flexor tendons of the fingers. Any condition that makes the area inside the carpal tunnel smaller or increases the size of the tissues within the tunnel can lead to symptoms of CTS. The carpal tunnel cannot expand so any condition that causes abnormal pressure in the tunnel can produce symptoms of CTS. And any increase in pressure within the carpal tunnel can reduce blood flow to the nerve, leading to loss of nerve function.
AFFECTED PATIENTS:
Carpal tunnel syndrome is very common in general population, particularly during pregnancy and in women around the age of 50. Manual workers, especially those who perform repetitive work (packaging, cleaning women, typing ...) are more likely to be affected by this pathology. Finally, those diseases that increase tendon thickness are most frequently associated with carpal tunnel syndrome: hypothyroidism, rheumatoid arthritis, amyloidosis, diabetes.
SYMPTOMS:
Symptoms of CTS is gradual tingling and numbness in the areas supplied by the median nerve. This is typically followed by dull, vague pain where the nerve gives sensation in the hand. The hand may begin to feel like it's asleep, especially in the early morning hours after a night's rest. Whether acute or chronic, pain associated with carpal tunnel syndrome may even spread up the arm to the shoulder. If the condition progresses, the thenar muscles of the thumb can weaken, causing the hand to be clumsy when picking up a glass or cup. If the pressure keeps building in the carpal tunnel, the thenar muscles may begin to shrink.
TREATMENT:
- First treatment is the use of a brace: A wrist brace keeps the wrist in a resting position decreasing the symptoms in the early stages of CTS. A brace can be especially helpful for easing the numbness and pain felt at night because it can keep your hand from curling under as you sleep. The wrist brace can also be worn during the day to calm symptoms and rest the tissues in the carpal tunnel.
- If these simple measure fail to control your symptoms or in severe cases, surgical treatment is needed. Surgical procedure is done to relieve pressure on the median nerve. By releasing the pressure on the nerve, the blood supply to the nerve improves, and most people get relief of their symptoms. The procedure is performed under locoregional anesthesia (without general anesthesia) and on an outpatient basis (you do not stay in the clinic). Surgery can be performed using the usual 2 cm hand incision technique, or by using the endoscopic technique with a small 1 cm incision.

AFTER SURGERY:
After surgery, the wrist is immobilized with a bandage for 3.4 days. It is important to move fingers from the day after the intervention. The duration of recovery varies according to the individual being in most cases immediate. If the nerve pressure has been going on a long time, the median nerve may have thickened and scarred to the point that recovery after surgery is much slower. A nerve recovers at the rate of one mm daily In manual workers, work reincorporation is usually possible 3 weeks after the intervention.
Cubital Tunnel Syndrome
WHAT IS THE CUBITAL TUNNEL SYNDROME?
Cubital tunnel syndrome is compression or irritation of the ulnar nerve in a tunnel on the inside of the elbow (where your 'funny bone' is). The ulnar nerve provides sensation to the little finger and part of the ring finger, and power to the small muscles within the hand.
SYMPTOMS
Cubital tunnel syndrome symptoms usually include pain, numbness, and/or tingling. The numbness or tingling most often occurs in the ring and little fingers. The symptoms are usually felt when there is pressure on the nerve, such as sitting with the elbow on an arm rest, or with repetitive elbow bending and straightening. Often symptoms will be felt when the elbow is held in a bent position for a period of time, such as when holding the phone, or while sleeping. Some patients may notice weakness while pinching, occasional clumsiness, and/or a tendency to drop things. In severe cases, sensation may be lost and the muscles in the hand may lose bulk and strength.
TREATMENT
- Changing the patterns of elbow use may significantly reduce the pressure on the nerve. Avoiding putting your elbow on hard surfaces may help, or wearing an elbow pad over the ulnar nerve and "funny bone” may help. Keeping the elbow straight at night with a splint also may help.
- When symptoms are severe or do not improve, surgery may be needed to relieve the pressure on the nerve. This can involve releasing the nerve, and moving the nerve to the front of the elbow.
De Quervain's Tendonitis
WHAT IS THE DE QUERVAINS TENDONITIS?
The De Quervain's tenosynovitis is an inflammation of the tendon sheath of the thumb (long abductor and short extensor) at the outer edge of the wrist. The inflammation causes the compartment around the tendon to swell and enlarge, making thumb and wrist movement painful. The cause of de Quervain's tendonitis is an irritation of the tendons at the base of the thumb, usually caused by taking up a new, repetitive activity. New mothers are especially prone to this type of tendonitis: caring for an infant often creates awkward hand positioning, and hormonal fluctuations associated with pregnancy and nursing further contribute to its occurrence.

SYMPTOMS
Pain over the thumb-side of the wrist is the main symptom. The pain may appear either gradually or suddenly, and pain is located at the first dorsal compartment at the wrist. Pain may radiate down the thumb or up the forearm. Hand and thumb motion increases pain, especially with forceful grasping or twisting. There may be an occasional "catching” or "snapping” when moving the thumb. Finkelstein test is always positive: the patient makes a fist with the fingers clasped over the thumb. The wrist is then bent in the direction of the little finger .This maneuver should be quite painful for the person with de Quervain's tendonitis.

TREATMENT
The goal is to relieve the pain caused by the irritation and swelling. It may be usefull resting the thumb and wrist by using a splint or doing Oral anti-inflammatory medication. A cortisone-type of steroid may be injected into the tendon compartment as another treatment option. Each of these non-operative treatments help reduce the swelling, which typically relieves pain over time. In some cases, simply stopping the aggravating activities may allow the symptoms to go away on their own. When symptoms are severe or do not improve, surgery may be recommended. Surgery opens the compartment to make more room for the inflamed tendons, which breaks the vicious cycle where the tight space causes more inflammation. Normal use of the hand can usually be resumed once comfort and strength have returned.

Trigger Finger
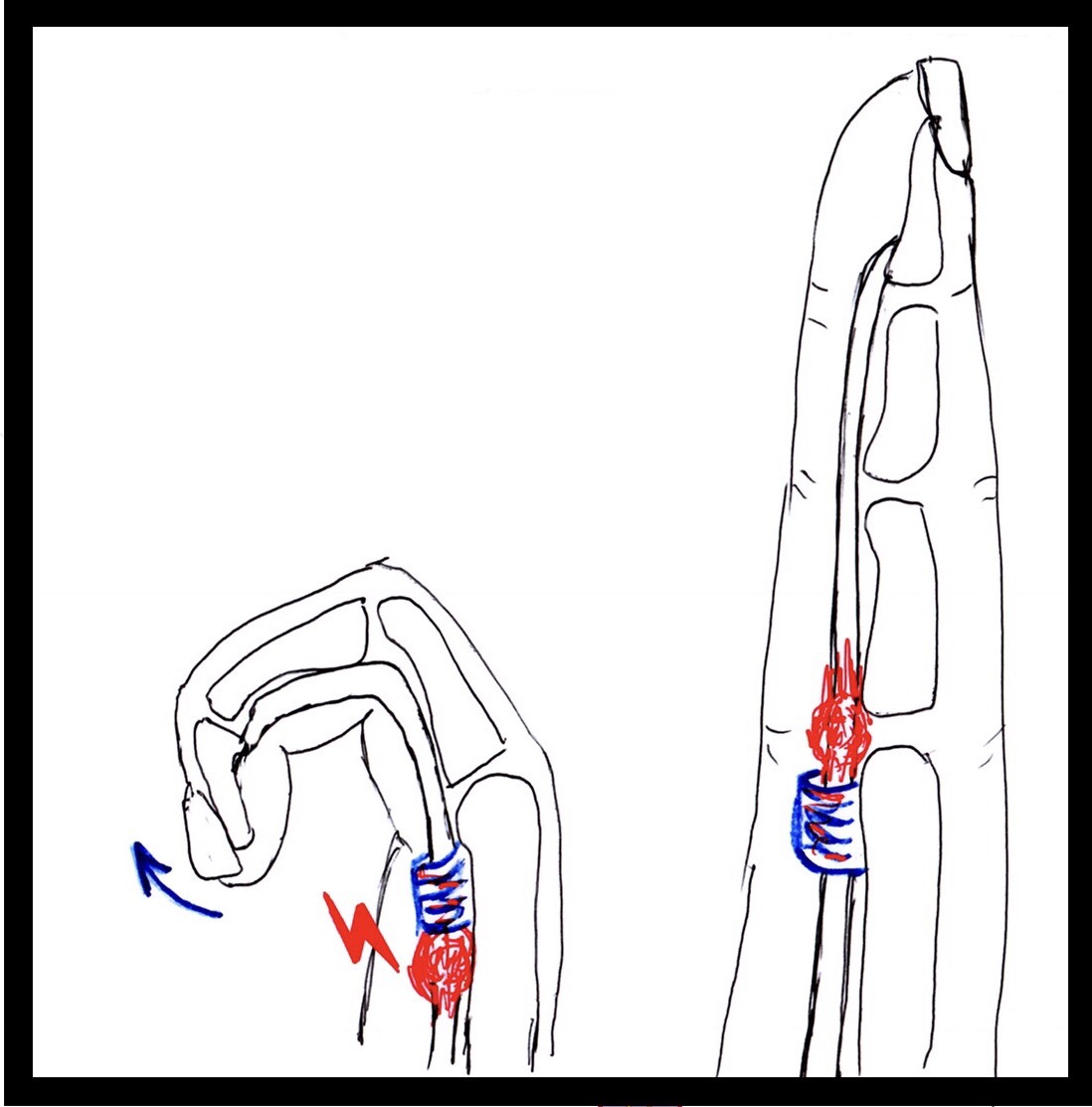
WHAT IS THE TRIGGER FINGER?
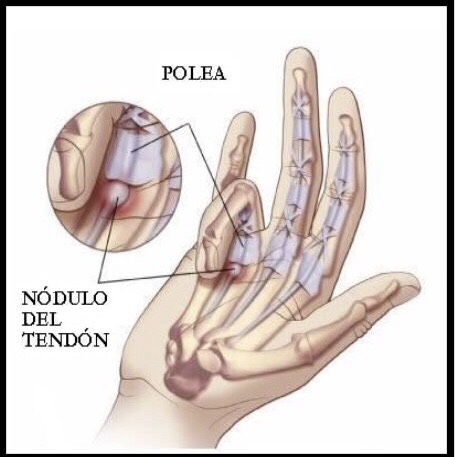
Stenosing tenosynovitis, commonly known as "trigger finger”, involves the pulleys and tendons in the hand
that bend the fingers. The tendons work like long ropes connecting the muscles of the forearm with the bones
of the fingers. In the finger, the pulleys are a series of rings that form a tunnel through which the tendons
must glide. Trigger finger occurs when the pulley at the base of the finger becomes too thick and constricting
around the tendon, making it hard for the tendon to move freely through the pulley. Because of the increased
resistance to the gliding of the tendon through the pulley, one may feel pain, popping, or a catching feeling
in
the finger. When the tendon catches, it produces inflammation and more swelling. Sometimes the finger
becomes stuck or locked, and is hard to straighten or bend.
As the disease progresses, the tendon may thicken and nodules may form, making it more difficult to pass
through the tunnel.
The trigger finger's cause is unknown.
It is more common in women than in men.
Its frequency increases in people between the ages of 40 and 60 years.
It is associated with diabetes and rheumatoid arthritis.
SYMPTOMS
Trigger finger may start with discomfort felt at the base of the finger or thumb, where they join the palm. This area is often tender to local pressure. A nodule may sometimes be found in this area.
TREATMENT
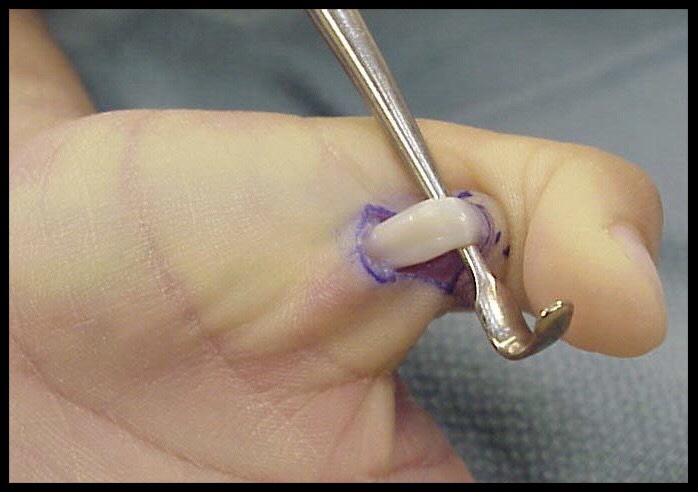
The goal of treatment in trigger finger is to eliminate the catching and allow full movement of the finger without discomfort. Swelling around the flexor tendon and tendon sheath must be reduced to allow smooth gliding of the tendon. Taking an oral anti-inflammatory medication may help. An injection of steroid into the area around the tendon and pulley is often effective in relieving the trigger finger. If non-surgical forms of treatment do not relieve the symptoms, surgery may be recommended. This surgery is performed as an outpatient, usually with simple local anesthesia. The goal of surgery is to open the A1 pulley at the base of the finger so that the tendon can glide more freely. Active motion of the finger generally begins immediately after surgery. Normal use of the hand can usually be resumed once comfort permits.
Dupuytren's Disease
WHAT IS THE DUPUYTREN DESEASE ?
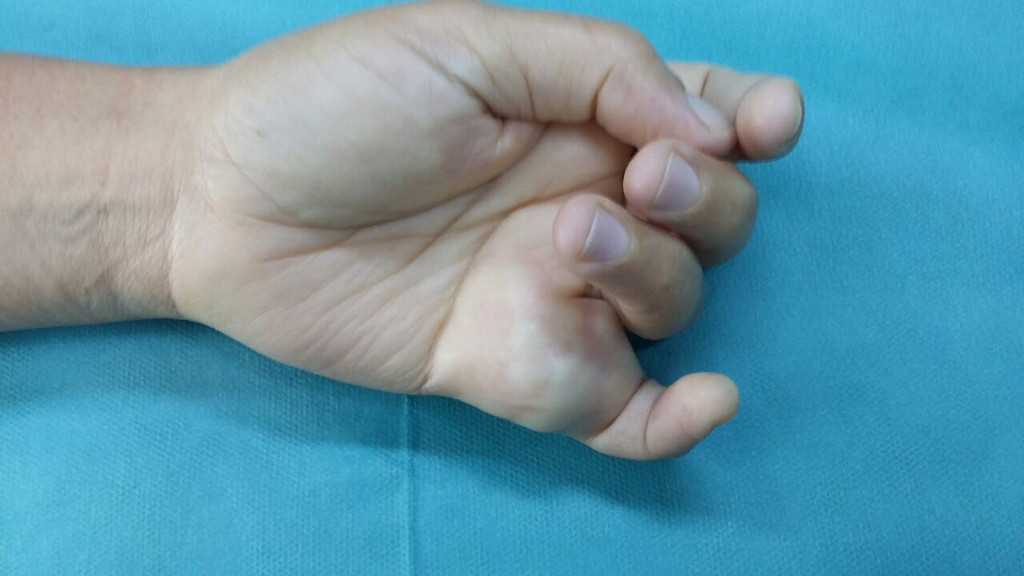
Dupuytren's disease is related to a thickening of a fibrous structure located under the skin of the palm of the hand and fingers. This thickening is accompanied by a retraction which limits the extension of the fingers and can infiltrate the skin. The retraction of the fingers is not accompanied by pain. Dupuytren's disease is more frequent in northern Europe and more often affects man than woman. Often, another member of the family also presented the disease (hereditary disease). Some medications or alcohol may promote this disease.
When is the surgery indicated?
The intervention can be considered from the moment when the patient can no longer lay his hand flat on the table. The treatments differ according to the nature and the importance of the lesions (deficiency of extension, condition of the skin).
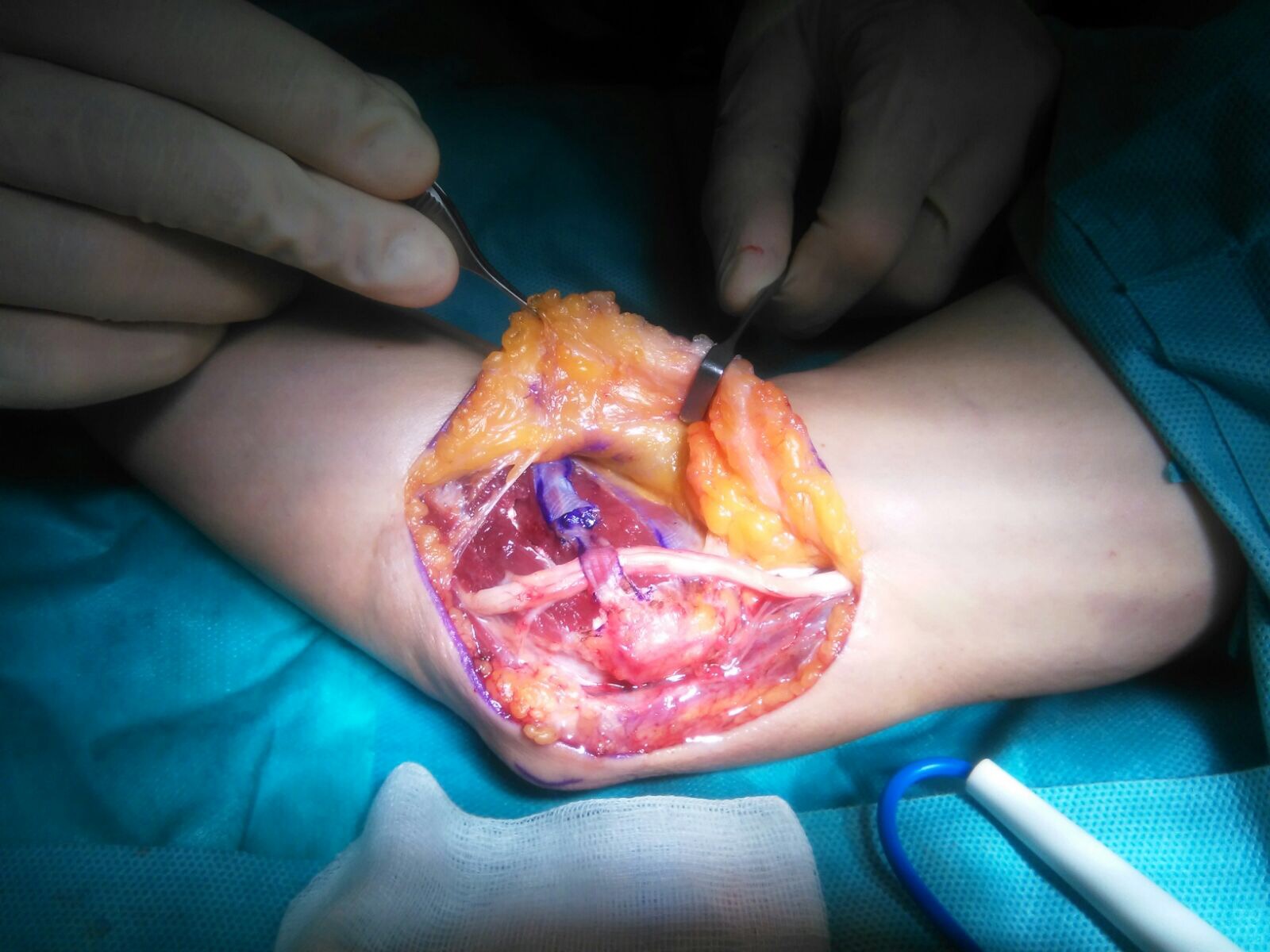
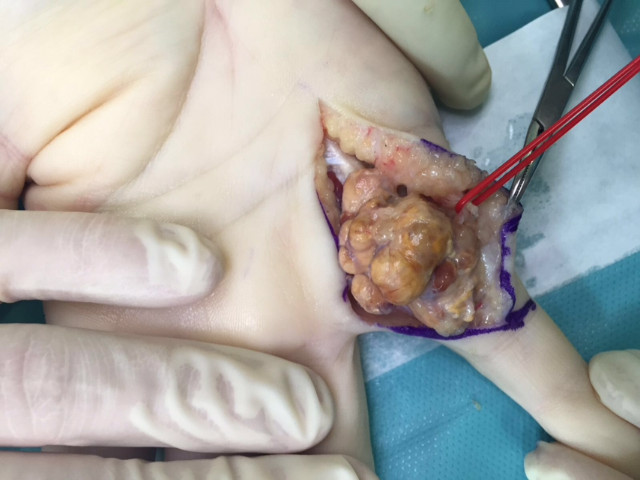
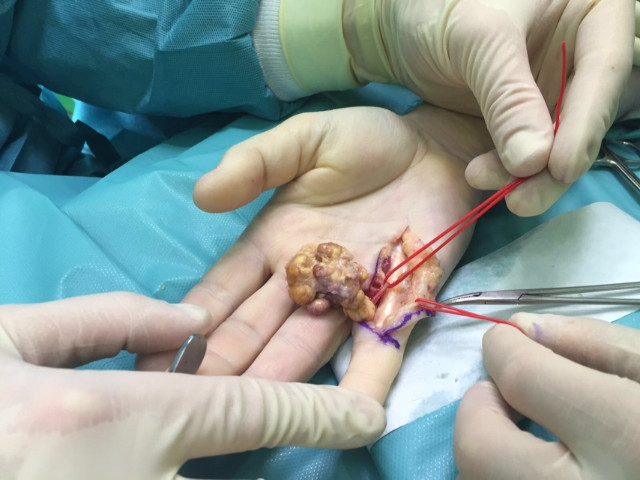
TREATMENT
- Regional Fasciectomy: This is the most used treatment. Zigzag incisions are made in the palm and along the fingers. This allow the removal of abnormal tissue responsible for the flexion of the fingers. These incisions take between two and three weeks to heal and will be thick for several months. Reeducation and wearing a splint to extend the fingers are very often necessary. Occasionally, skin grafts may be needed to replace damaged skin. This makes this operation tricky and the proximity between abnormal tissues and vessels and nerves. Dissection and ablation of abnormal tissues in contact with vessels and nerves is difficult and should always be done with microsurgical glasses.
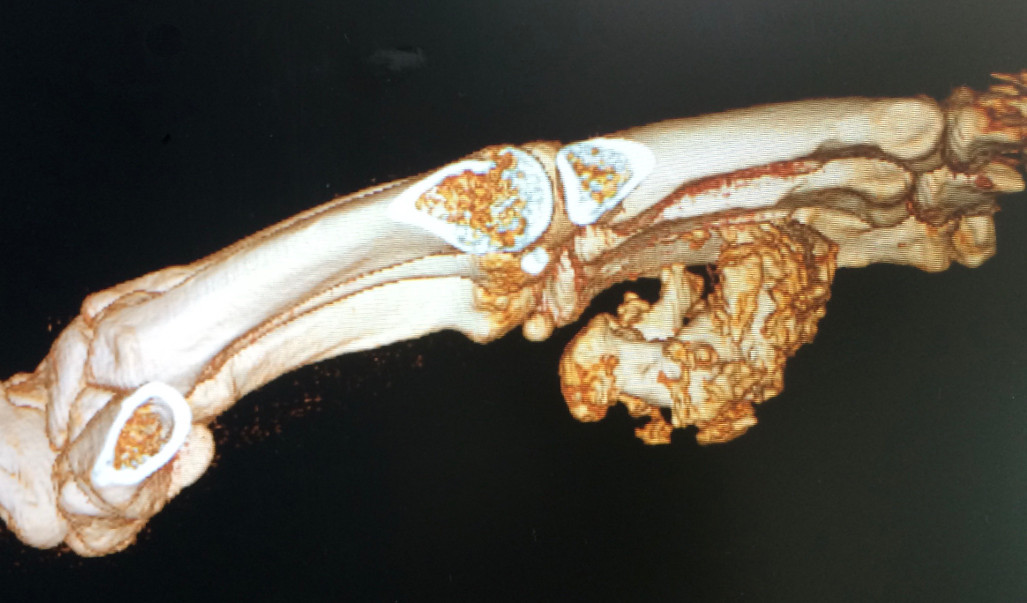
- Case 1




- Case 2
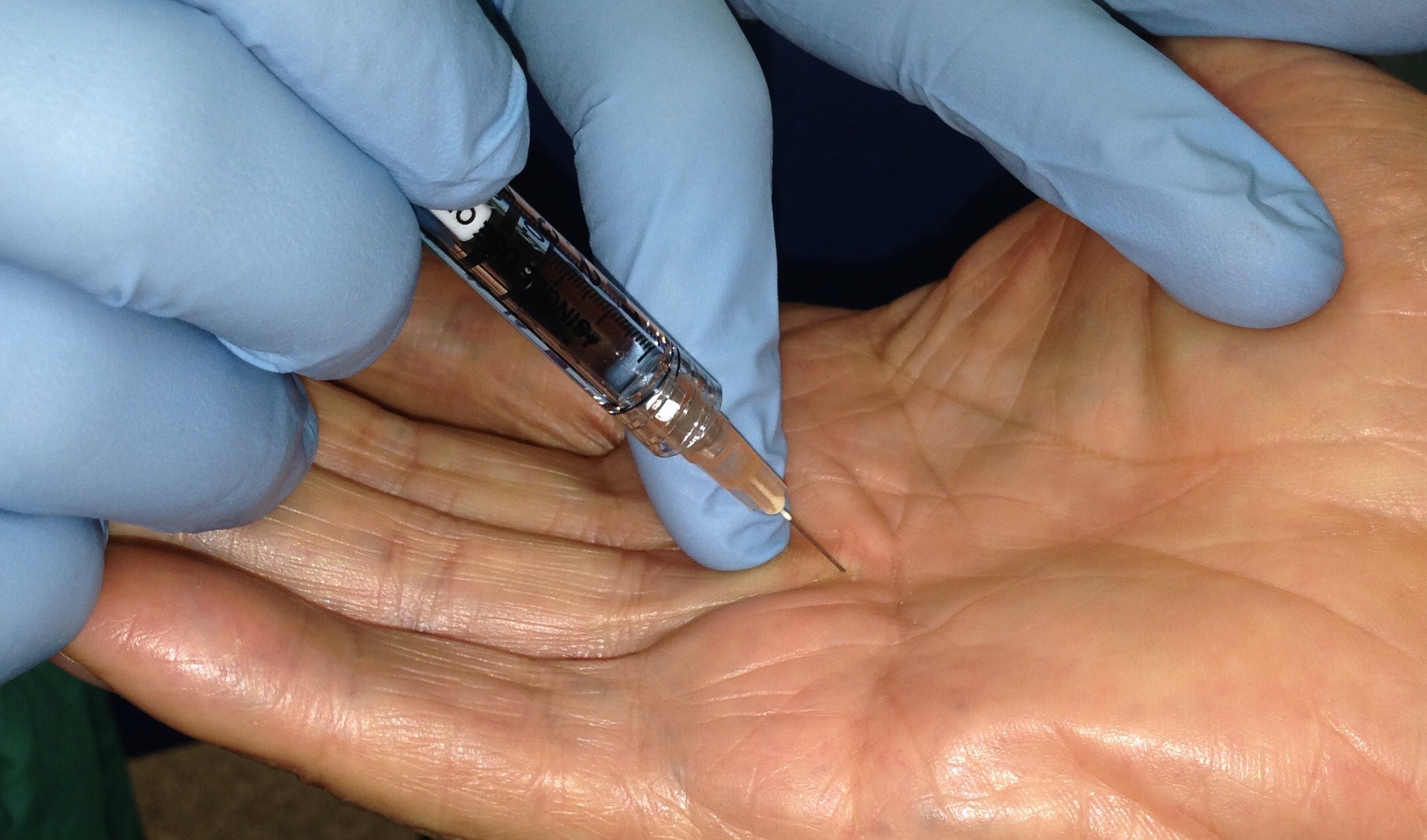
- Injection of Clostridium Histolytcum Collagenase: A product is injected which will dissolve the
pathological tissues within a few days. This new method can be carried out in the same cases as
an aponeurotomy, but more often in easy cases or patients with lot of morbidity.


Rheumatoid Arthritis
WHAT IS THE RHEUMATOID ARTRHITIS?
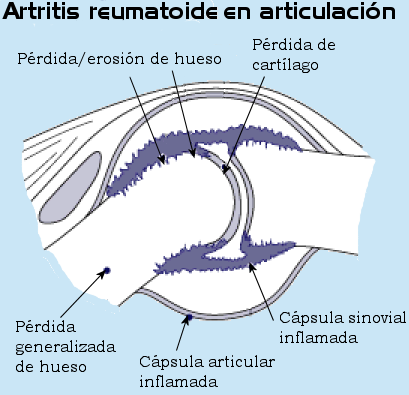
Rheumatoid arthritis affects the cells that line and normally lubricate the joints. This is a systemic condition which affect the whole body, and may affect multiple joints, usually on both sides of the body. The synovium becomes inflamed and erodes the cartilage and bone. The swollen tissue may also stretch the surrounding ligaments resulting in deformity and instability. The inflammation may also spread to the tendons, this resulting in stretching out of and ruptures of the tendons. Rheumatoid arthritis of the hand is most common in the wrist and the finger MP and PIP joints
CAUSES
RA is a systemic (whole body) autoimmune disease. Some genetic and environmental factors impact on the risk for RA. Rheumatoid arthritis affects 0.25% of the general population, and women three times as often as men. This is the most common chronic inflammatory rheumatism. Although the disease can occur at any age, the first symptoms usually occur around 40 to 60 years.
SYMPTOMES
Rheumatoid arthritis affects the joints (synovial tissue). It is a systemic disease, which means that it can affect many joints, usually in a symmetrical manner. The synovial joint becomes inflamed, and erodes the cartilage and bone. This hypertrophic synovium, due to its growing volume, will also occupy more space than available within the joint. This will cause tensioning of the ligaments and the articular capsule surrounding it and distort them, which will result in deformation and instability of the joints. Inflammation progressively erodes the tendons and can lead to their rupture. This rupture can also occur by a phenomenon of friction of the tendons on the deformed bone structures. Rheumatoid arthritis of the hand is more commonly seen in the joints of the wrist and fingers. The joints that are most often affected by rheumatoid arthritis are the hands, wrists, feet, ankles, knees, shoulders and elbows. The disease usually causes symmetrical inflammation of the joints of the body. The symptoms are:
- Pain.
- Morning stiffness.
- Inflammation of the joints.
- Decreased movement.
- Deformity of the joints.

TREATMENT
Treatment is first and foremost medical. Anti-inflammatory treatments, oral corticosteroids or cortisone injections may be prescribed. Various treatments are available today, including methotrexate, cyclosporine, and new drugs (biological treatments) that inhibit the body's immune system to reduce inflammation and pain. It is based above all on the use of ortheses or custom- made splint. When sufficient medical treatment becomes insufficient to alleviate the pain, or if there is a tendon rupture, or deformation of the fingers, surgical treatment may be considered. Preventive surgery includes removal of nodules and release of pressure on the tendons by removing degenerated tissue or bone irregularities that can erode the tendons. If a tendon is ruptured, it must be repaired with a transfer or a tendon graft. Surgical treatments of arthritic joints include resection of inflammatory synovial tissue, joint replacements, and joint fusion. Specific procedures depend on a variety of factors, including the type of joint involved, the severity of the condition, and the condition of the adjacent joints.
Thumb Arthritis
WHAT IS THE ARTHRITIS OF THE THUMB?
Thumb arthritis is common with aging, and occurs when cartilage wears away from the ends of the bones that form the base of the thumb joint also known as the carpometacarpal joint.
SYMPTOMS
The most common symptom is pain at the base of the thumb. The pain can be aggravated by activities that require pinching, such as opening jars, turning door knobs or keys. Severity can also progress to pain at rest and pain at night. In more severe cases, progressive destruction and mal-alignment of the joint occurs, and a bump develops at the base of the thumb as the metacarpal moves out of the saddle joint. This shift in the joint can cause limited motion and weakness, making pinch difficult.
TREATMENT
Initial thumb arthritis will usually respond to non-surgical care. Arthritis medication, splinting and cortisone injections may help alleviate pain. A hand therapist might provide a variety of splints which can be used while sleeping or during activities. Patients with advanced disease or who fail non-surgical treatment may be candidates for surgical reconstruction. A variety of surgical techniques are available that can successfully reduce pain. Surgical procedures include arthroplasty, joint fusion, and other techniques such as the use of a "tight rope" procedure...
- Case 1 (Thumb arthroplasty)


- Case 2 (tightrope procedure)


Mucoid Cyst

WHAT IS THE MUCOID CYST?
These are small benign swellings, located on the back of the last articulation of the fingers (distal inter-phalangeal joint) near the nail. These are cysts of articular origin, filled with a translucent, viscous fluid. They often develop on osteoarthritic joints. The tendency of these cysts is to extend, either at the depth where they compress and deform the nail, or in area where they are fistulized.
DIAGNOSIS:
The tumefaction, located on the dorsal surface of the finger just upstream of the nail, is the main sign. The skin can be very fine, almost transparent. The nail is sometimes deformed longitudinally, mostly recessed, over the entire length. The underlying IPD joint is most often osteoarthritis, causing pain, joint deformation and limitation of mobility. Finger radiography is necessary to find underlying osteoarthritis.
TREATMENT
Aspiration of the contents are useless, as recidivism is the rule. Bulky cysts, fistulized, or complicated by nail deformity should be operated. When the skin is fragile or pierced, it is removed to be covered by a skin graft (taken from the hand or forearm) or a flap (the neighboring skin is peeled off and turned over the loss of substance). It is also necessary to remove the bone protrusions from the joint (parrot beaks). Nothing is done on the deformed nail: after the removal of the cyst, the nail regrowth will often make the deformation disappear. If the joint is deformed and painful, a blockage of the IPD joint (arthrodesis) can be achieved.
Tendons Injury
WHAT ARE TENDONS?
Tendons are tough cords of tissue that connect muscles to bones allowing you to make a wide range of movements. There are two types of tendons in the hand: Extensor tendons run from the forearm across the back of your hand to your fingers allowing you to straighten your fingers. Flexor tendons run from your forearm through your wrist and across the palm of your hand, allowing you to bend your fingers. Wounds on the hand and fingers are particularly serious and complex because of the importance of structures that can be injured. A small-looking wound may be associated with a major nerve, vascular, or tendon injury.
CAUSES OF TENDON INJURY
In addition to cuts on the arm, hand, or fingers, certain sports activities can cause flexor tendon injuries. These injuries often occur in football, and rugby. "Jersey finger" is one of the most common of these sports injuries. It happens when a player grabs another's jersey and the finger gets caught and pulled. The tendon is pulled off the bone. Certain health conditions (rheumatoid arthritis) weaken the flexor tendons and make them more likely to tear.
SYMPTOMS
The most common signs of a tendon injury include an open injury such as a cut and an inability to bend or extend one or more joints of your fingers. This can also happen without warning or injury and the person may simply notice that one or more finger suddenly no longer moves.
DIAGNOSIS
The examination of the hand and fingers are the key of the diagnosis. Anyone suspecting a tendon injury should be evaluated by a surgeon specializing in hand surgery. This should occur as soon as possible as the functional outcome after repair is affected by the length of time between injury and repair.
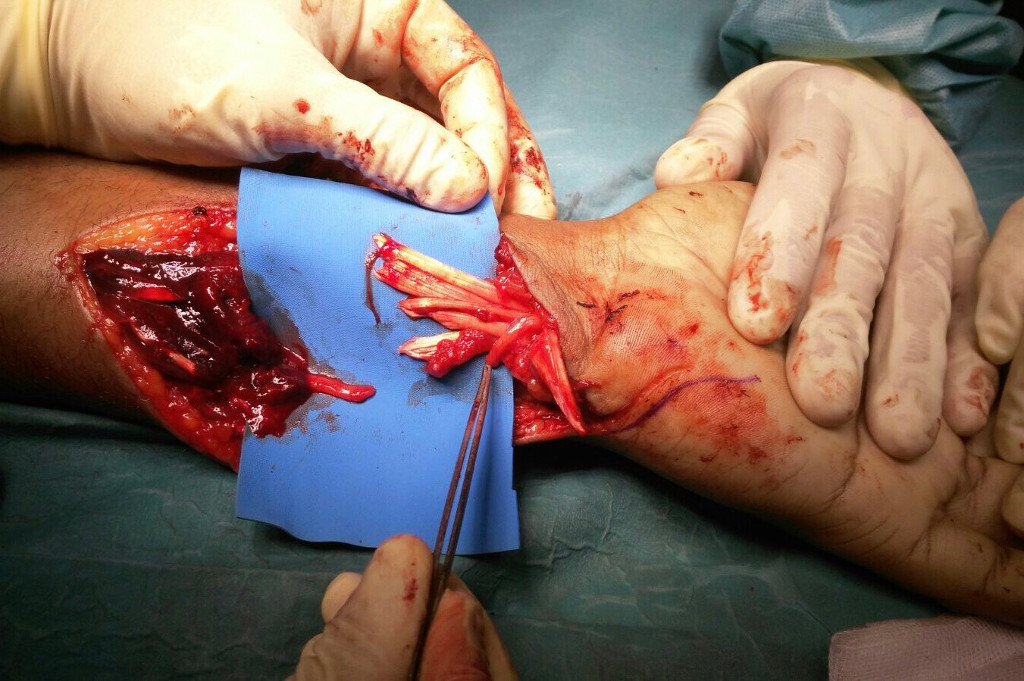
TREATMENT
Tendon injuries are repaired surgically. This repair involves bringing the two tendinous stumps together and suturing them according to specific techniques so as to ensure the best slip while obtaining maximum strength. This procedure must be protected by a splint and a rehabilitation protocol will be established immediately. Healing of the tendons may be the cause of adhesion formation between the tendon and the underlying bone structure, limiting tendon gliding. The scar tissue that forms can prevent flexion and full extension of the finger. Surgery to release the tendon from these adhesions can sometimes be useful in cases of significant loss of mobility.


Hand Tumors
WHAT ARE HAND TUMORS?
Most tumors of the hand are benign. Cancers are rare. These tumors can develop from the skin, muscle, fat, tendons, nerves vessels or bone. The most common types of hand tumors are ganglion cyst and giant cell tumors of the tendon sheath. A ganglion cyst is a fluid filled mass that is frequently found in the joints of the hand or wrist. Giant cell tendon sheath tumors present as a solid lump on the hand or finger. While these types of tumors are not cancerous, they can be extremely painful and decrease hand function.


CAUSES
Cause of tumors of the hand is unclear, however trauma is thought to play a role in some. Repetitive motion injuries can cause inflammation leading to abnormal growth of cells. Occasionally skin cells or a foreign body can become trapped within the tissues resulting in tumor growth encapsulating the debris. Over time Arthritis can cause boney growths called bone spurs to form which can be hard and painful. While most Hand Tumors are benign the likelihood of cancer is a rare but real possibility.
SYMPTOMS
Most Hand Tumors present as a visible lump on the wrist; hand or fingers. They can form gradually over time or appear suddenly on or below the surface of the skin. They may be soft to firm and may or may not move on palpation. Many tumors are painless and go undiagnosed until they actually interfere with hand function or become large in size. Tumors growing near a nerve or on the bone can be extremely painful and so are usually diagnosed earlier. Depending on location a hand tumor may affect joint mobility or may just be aesthetically displeasing.
DIAGNOSIS
The physician will require a detailed history including traumatic injuries, occupational hazards and family history. A complete physical examination of the extremity will then be performed. X ray, MRI (magnetic resonance imaging) and ultrasound are used to visualize the soft tissues for abnormalities.
TREATMENT
Most hand tumors will require surgical excision to completely remove the mass and prevent recurrence. Once the mass is removed it is sent to a lab for pathology. This is the only way to determine whether the growth is benign or malignant. If non-cancerous, no other treatment (except possibly hand therapy) is required as the lump has already been removed.
- Case 1

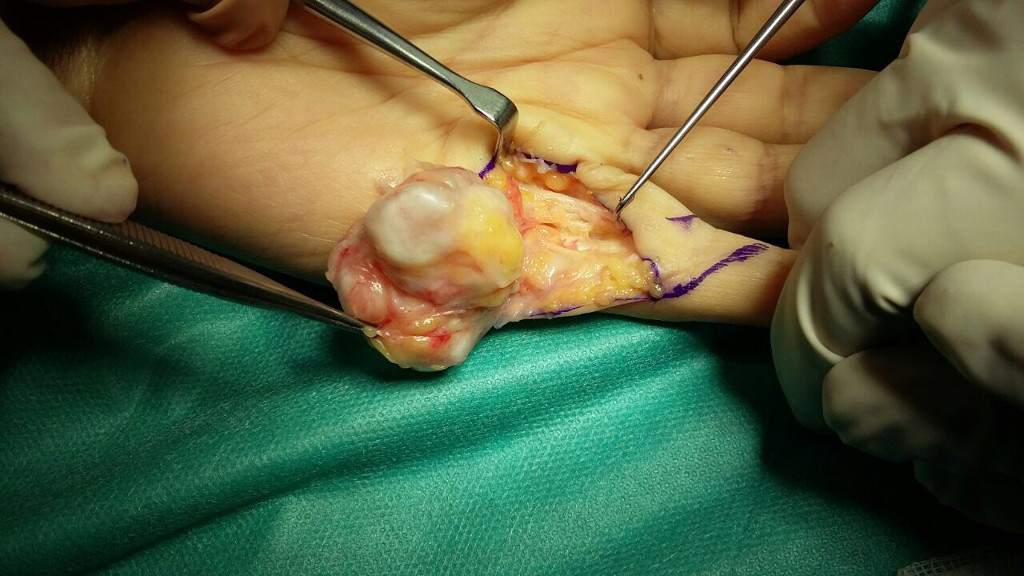

- Case 2

Mallet Finger
WHAT IS THE MALLET FINGER?
Mallet Finger is a deformity in which the fingertip bends downward at the end joint and can no longer be straightened. Occasionally it may associate a fracture of the base of the first phalanx

CAUSES
Mallet Finger is sometimes called Baseball Finger as it a common fast ball injury. While routinely seen in athletes, this deformity can also occur from crush injuries, jammed fingers or even a knife wound. Whether the extensor tendon is cut or the bone is fractured at the site of tendon attachment the result is the same.
SYMPTOMS
The mallet finger deformity will be evident at the time of injury. The distal phalanx will not straighten without physical assistance. Various degrees of pain, swelling, and tenderness will be present dependent on whether or not the bone is fractured.
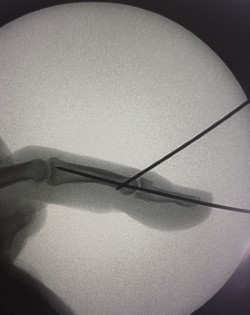
DIAGNOSIS
Mallet Finger is easily diagnosed due to its unique presentation. X-rays will be ordered to assess for the presence and extent of bone fracture. This aids in determining the appropriate treatment plan.

TREATMENT
Most cases of Mallet Finger can be treated without surgery, as long as there are no large bone fractures. A special finger splint may be applied to hold the digit in proper alignment while the tendon heals. The splint is worn continuously for 6 weeks, then at night for an additional 6 weeks. Surgical repair may be considered when mallet finger injuries have large bone fragments or joint mal-alignment. In these cases wires or even small screws are used to secure the bone fragment and realign the joint or to do a temporary fusion of the distal interphalangeal joint.